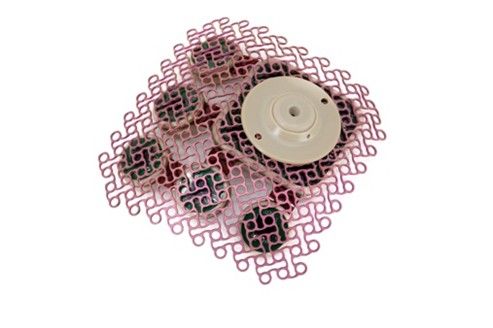
Glioblastoma is one of the most aggressive and deadly forms of brain cancer, notorious for its resistance to treatment and devastating prognosis. But a breakthrough approach from the company Carthera is offering new hope to patients with recurrent glioblastoma (rGBM) through an ongoing clinical trial.
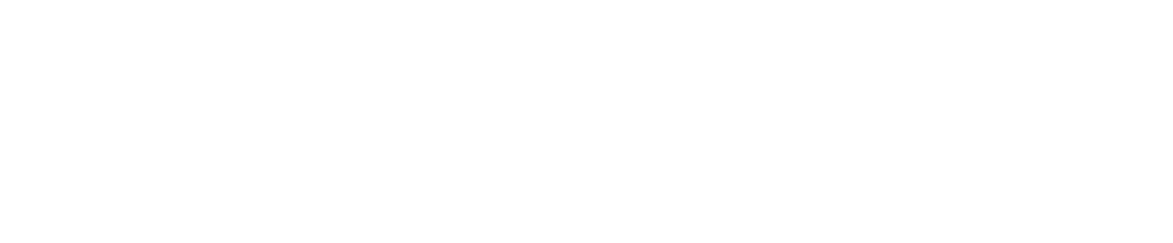
At the heart of Carthera’s innovation is a device called the SonoCloud—an implantable ultrasound device that is surgically placed in the skull, replacing a small section of bone. Its mission? To temporarily open the blood-brain barrier (BBB), a tightly controlled gateway that protects the brain from harmful substances but also blocks most therapeutic drugs. By briefly disrupting the BBB with pulsed ultrasound, SonoCloud significantly enhances the delivery of cancer-fighting drugs to brain tumors. A 2023 study in Lancet Oncology demonstrated a 4-6-fold increase in brain concentrations of chemotherapy drugs following SonoCloud treatment.
In a recent episode of the PsyDactic podcast, Michael Canney Ph.D., Chief Scientific Officer at Carthera, explained the science behind this approach. “The blood-brain barrier is a major obstacle in treating brain cancers,” he said. “SonoCloud enables us to bypass that barrier safely, repeatedly, and in a controlled fashion.” The device uses low-intensity pulsed ultrasound in combination with microbubbles injected into the bloodstream. When ultrasound waves interact with these microbubbles, they oscillate, creating temporary openings in the BBB that close within a few hours. Initial results, published last year in Nature Communications, have been encouraging, showing that the technology is both safe and feasible over multiple treatment cycles.
Carthera’s pivotal trial—known as SONOBIRD, is underway at over 40 clinical sites in Europe and the United States. The trial is testing whether adding SonoCloud-mediated BBB opening to carboplatin chemotherapy can extend survival for patients at first recurrence of grade IV glioblastoma and eligible for re-surgery, in comparison with standard-of-care treatments (eg lomustine or temozolomide).
What sets the SonoCloud trial apart is its focus on repeatability and integration into clinical workflows. Unlike more invasive or one-off techniques, SonoCloud is designed for chronic use, with patients undergoing BBB opening every three weeks when they receive chemotherapy. The procedure itself takes just a few minutes and is done in an outpatient setting.
“It has been a privilege to offer this trial to patients with recurrent glioblastoma,” said Dr. Brian Gill, assistant professor of neurosurgery at Columbia University Irving Medical Center in New York. “The underlying concept is highly promising, device implantation has proceeded smoothly and patients have shown strong interest in participating.”
While the current trial focuses on glioblastoma, Carthera is exploring applications in other diseases, including brain metastases and neurodegenerative disorders. The ability to open the BBB on demand could transform drug delivery for a wide range of central nervous system diseases.
If successful, SonoCloud could mark a paradigm shift in how brain diseases are treated. “We’re not just developing a device,” said Dr. Canney. “We’re opening a door to make therapies work better in the brain.”
For patients with rGBM, that door—once firmly closed—may finally be opening, offering renewed hope.